What Is A Gastrointestinal Fistula And What Causes It?
A fistula occurs when a connection is formed between one organ and another structure, usually as a result of injury. A gastrointestinal fistula is very common in patients with Crohn’s disease. Up to 35% of them will get at least one at some point in their lives.
On the other hand, this health problem is also common in patients who have undergone abdominal surgery. According to studies (English link) creates up to 85% of fistulas as a side effect of these interventions. If you want to know everything about gastrointestinal fistulas and how to deal with them, you’ve come to the right place!
Types of Gastrointestinal Fistulas
Scientific studies (Spanish link) classify fistulas according to their site of occurrence, so they can be external or internal. Internal fistulas connect two organs together, while external fistulas communicate directly or indirectly with the body surface.
In addition, depending on the number of connections they generate, they can also be simple or complicated. Based on their location, 4 different types of gastric fistulas can be distinguished:
- Esophagus, stomach and duodenum.
- In the small intestine.
- In the gut.
- Any of the above with a wall defect greater than 20 square inches.
The last term is striking. Fistulas are openings that allow fluids to escape from the gastrointestinal tract. Based on this parameter, a fistula can be low-flow (discharges less than 500 milliliters per day) or high-flow (discharges more than 500 milliliters per day).
What are the symptoms of a gastrointestinal fistula?

The drugs.com portal lists some of the most common symptoms of the presence of a gastrointestinal fistula in patients. Some of the most common causes include:
- Abdominal pain or gassy indigestion.
- Diarrhea.
- Weight loss, nausea and vomiting.
- Heartburn.
- Fluid that leaks through a wound in the abdomen.
With an internal fistula, the patient may also experience rectal bleeding, inflammation, nutrient malabsorption, dehydration, and a worsening of underlying health conditions. On the other hand, some fistulas do not generate any symptoms. It all depends on the above parameters and on the state of health of the individual.
Any complications
If a person experiences heavy rectal bleeding, uncontrolled vomiting and nausea, or abdominal distension, they should seek urgent medical attention. Some fistulas can be life-threatening if accompanied by a bacterial infection in the surrounding tissue.
Despite advances in medicine, research shows that 25 to 50% of patients with enterocutaneous fistulas eventually die. However, this data is not entirely representative as we are mostly talking about people who are already in poor health.
Main causes of a gastrointestinal fistula
Medical studies investigate the main causes of gastrointestinal fistulas. In the following paragraphs, we will briefly tell you about their findings.
Operative Procedures
As mentioned above, 75-85% of gastrointestinal fistulas are the result of a complication after abdominal surgery. It is difficult to get a specific figure because it depends on many factors, but all authors agree on the same thing: more than half of all fistulas develop in the postoperative period.
Diverticula and diverticulitis
The occurrence of diverticula that seriously affect the colon can also cause the development of fistulas. These are located as connections to intra-abdominal organs, for example the bladder.
Crohn’s disease
Crohn’s disease causes long-term chronic inflammation of certain parts of the digestive tract. This leads to abdominal pain, fever, fatigue, constipation and blood in the stool. Up to 35% of people with this pathology develop one or more fistulas in their lifetime.
Malicious Processes
The occurrence of cancerous tumors in the intestine and adjacent organs promotes fistula formation. Radial expansion of a mass in the mucosa of the digestive tract and destruction of normal tissue favors the formation of fistulas.
How can a gastrointestinal fistula be diagnosed?

The United States National Library of Medicine lists some of the most effective diagnostic methods for detecting a gastrointestinal fistula. These include:
- Esophagography: A series of X-rays taken to assess the condition of the esophagus, stomach, and small intestine. The fistula is immediately searched for.
- Barium enema: A special contrast dye of the colon that includes the colon and rectum.
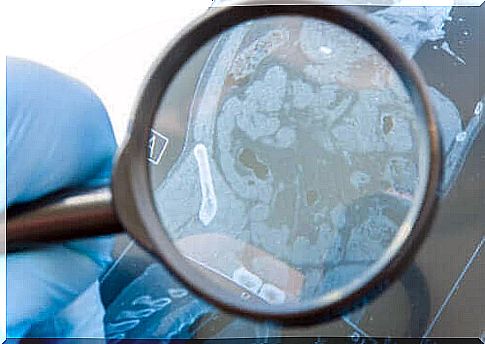
- CT scan: This tool is used to look for fistulas in the abdominal cavity between the intestinal loops or areas where previous infections have occurred.
- Fistulogram: Uses a form of real-time X-ray, fluoroscopy, and contrast material (barium-based), to generate images of an abnormal passageway in the body.
While all diagnostic methods are suitable, the fistulogram is the technique that provides the most relevant medical information. The fistulogram , in addition to detecting the fistula itself, allows doctors to evaluate the condition of the lesion and its extension.
Available treatments
There are two variants of treatment: conservative and surgical. In the first case, doctors usually prescribe antibiotics to prevent the development of serious bacterial infections. In addition, if the fistula is due to Crohn’s disease, the patient should receive immunosuppressants.
Other conservative approaches include the use of fibrin sealants to close the fistula in a minimally invasive manner and intravenous feeding of the patient while it heals. The success rate of this approach is not very high, so it usually results in surgical excision of the affected area.
A Gastrointestinal Fistula: A Complication of an Underlying Problem
In conclusion, we can state that a gastrointestinal fistula is a difficult clinical problem to treat. It usually arises as a result of a previous complication, surgery, or long-term bowel disease.
The prognosis therefore depends on the primary health problem and on the patient’s personal situation. The quality of life is strongly affected and can also interfere with the treatments that the patient undergoes.